Double-Mastectomy w/Reconstruction: Surgery Plans
After a false start back in June, we are back on track with a surgery schedule (assuming there are no hiccups between now and then--and let's be honest, this entire year has been an awful case of the hiccups).
I recently met with my breast surgeon (who will do the double-mastectomy) and plastic surgeon (who is in charge of the reconstruction process) and we have a surgical plan and a date -- though I hesitated to give anyone the date in the 2020 world of cancellations and rescheduling.
But here it is: The planned surgery date is Monday, November 2nd, 2020. Its the date I would have chosen if I could have picked it myself, which makes me think it'll probably change. They didn't think it was likely to change, and so we'll plan for that, but clearly I've been jaded by making useless "plans" this year.
As I describe the surgery plan, first you should know that I was given the option of a lumpectomy and radiation, a single mastectomy, or a double-mastectomy. I did not want a lumpectomy because it would leave me lopsided, or require a partial reconstruction with body tissues or implants. I also wanted to avoid radiation if possible, and eliminate the potential for having to have a mastectomy further down the road if recurrence were to happen. My mentality was just do it all now, make them even, and let's try to move on.
Once I decided on a double-mastectomy, I could then choose whether I wanted to do a nipple and skin sparing mastectomy (keeping the nipple and skin envelope for implants) or a simple mastectomy (taking the breast tissue, nipple, and skin envelope and then later reconstructing or tattooing nipples). As explained to me, the medical chances for recurrence were minimal in one option over the other, so it was truly my choice to do whatever I was most comfortable with doing.
Both my oncologist and my breast surgeon said the main goal in deciding is to do what would make me feel most assured moving forward and not look back in 6 months and wish I had done something different. For some people, that means keeping your own natural breasts and monitoring them regularly with mammograms, keeping a watchful eye on any recurrence of the original cancer or other breast cancers. For others, it means removing all the breast tissue, knowing if recurrence were to happen, it wouldn't be local in the breast, which would require a mastectomy at that point (if the cancer were to return in the breast and not elsewhere in the body).
I fell somewhere in-between. Because of the location of my tumor, the fact that it was not in my lymph nodes, and I tested negative for the BRCA1 gene mutation, I have the option of a nipple and skin-sparing mastectomy That means that I can keep my natural "look" with an implant placed inside the current skin pocket. Obviously it isn't quite that simple, but that's the gist.
This procedure does leave a tiny bit of breast tissue behind the nipple, where cancer could technically recur. But, by keeping that little bit of tissue, I will be eligible to continue to get regular mammograms to monitor any changes (which would not be done if all the tissue was removed as in a simple mastectomy). So, I get most of the assurance that the breast cancer can't recur locally and then require a mastectomy in the future, plus the regular monitoring of any new or recurrent local cancer through mammograms, and I get to look "mostly" like my old self when reconstruction is complete. So that's where I've landed. In 6 months, could I regret keeping my nipples? Maybe, and only time will tell. But I felt like I wouldn't regret taking all the breast tissue now, eliminating the need for another surgery down the road if mastectomy then became a must rather than a choice.
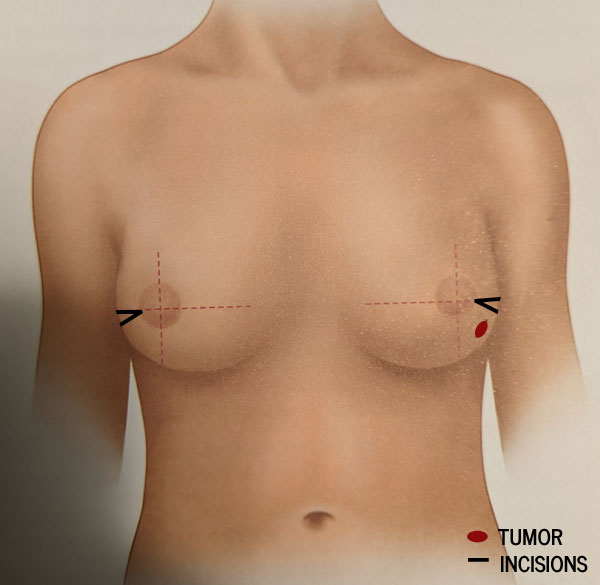
Next, we could start talking about the actual surgery. My breast surgeon describes the mastectomy as a small triangular incision at the sides of my breasts, removing just a tiny bit of skin near where the tumor on the left side was. She'll then scoop out and remove all the breast tissue underneath the skin and behind the nipple, which goes all the way up toward my collarbone. I can't imagine that's a pleasant feeling. Ouch.
She will also remove and test the nearest sentinal nodes (the first few lymph nodes where a tumor drains) and we hope that's all the lymph nodes she has to take. The more nodes they have to take, the higher chance I have to deal with lymphedema, which can be a permanant condition. Since this is on my dominant (left) side, that could potentially be pretty devastating for me. But since my earlier lymph node biopsy was negative, and we're pretty certain the tumor has shrunk down to indetectible on the mammogram, I'm feeling pretty good about what they'll find and have to take.
Then all of the tissue from both sides will be tested by pathology and I will get results back (probably not immediately) telling whether there were any cancer cells still present or anything else concerning in the chest wall or lymph nodes, and whether I will need any further treatment after surgery.
Next the plastic surgeon comes in to do his part -- the first phase of reconstruction. I've chosen to have silicone implants in a two-phase process involving temporary saline expanders inserted over the chest muscle and held in place with a processed "skin subsitute" material that forms a sling and helps hold the implant in place. Then the expanders are gradually filled with saline over a period of weeks or months to stretch your skin to the desired size. Then the expanders will be removed and replaced with permanent implants in a second surgery a few months later. This process is done in two steps to let your body settle and heal from the mastectomy, so you can have a little more say in the size of implants you end up with, and to make sure the tissue is all strong and healthy enough to support the implants and there are no other complications.
He gave me about a 25% chance that if everything looked strong and healthy I could wake up from surgery with the permanent implants already in place and skip the expander process. I'm not counting on that, but boy would that be great to avoid the process that many people have lots of compliants about. I've heard the expanders can be lumpy and hard and uncomfortable and the expanding process can be painful, etc. So, if I can safely avoid that and a second surgery -- I'm in favor. But, it sounded like that's not their usual mode of operation and a more conservative and slower process generally goes better with less complications.
Incidentally, I did not consider a flap surgery to use tissue from my own body (hips, belly, back or thighs) for reconstruction because 1) I don't have that much to give in those areas, 2) it's a much more difficult surgery and 3) I wanted to leave that as an option many years down the road, should I decide to remove whatever implants I get.
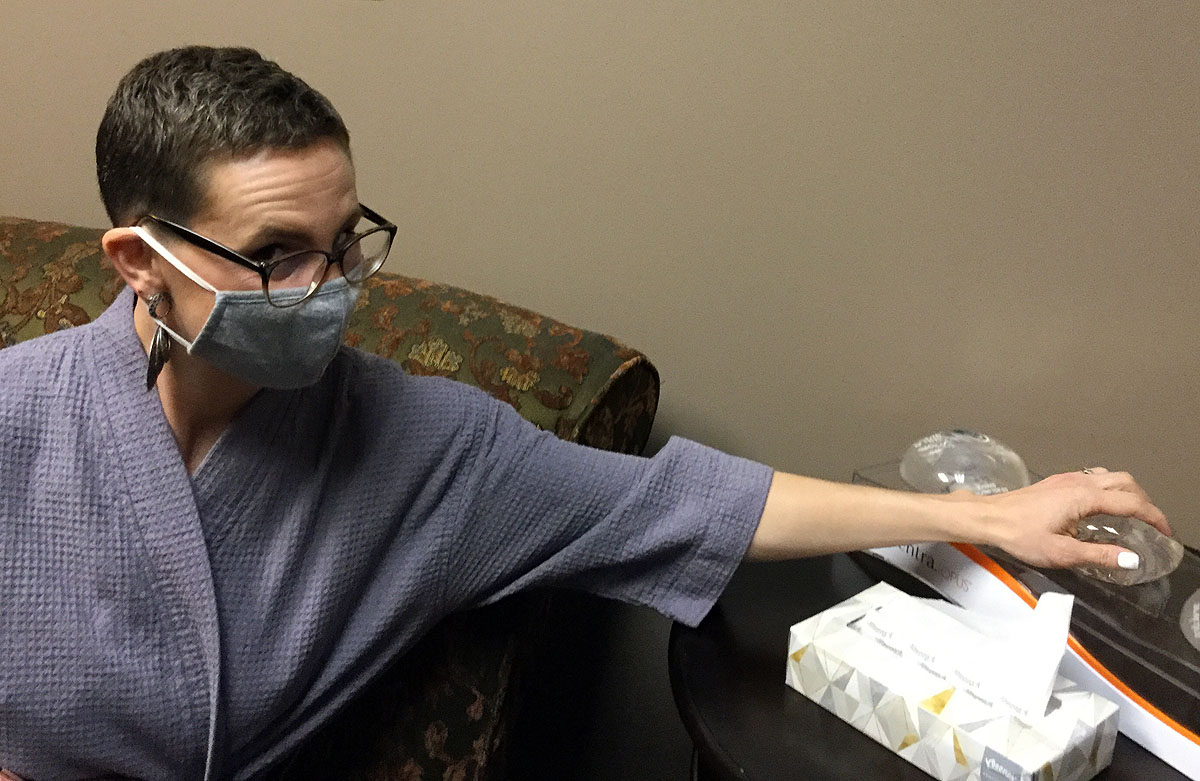
So what size will I get? I don't really know, and a lot of it will be determined by the fact that I am doing a nipple-sparing mastectomy. He said "we are at the mercy of where they point." Okay, then--Add that to list of things I never thought I'd hear! I told him, "I'd like to be a little bigger than I currently am, but not so big it's all people notice when I walk in a room," and his nurse laughed. We figure she's seen some excessively large requests! In all seriousness though, because there will be no breast tissue surrounding my implants, if I were to gain or lose weight, my breasts would stay exactly the same size. Since it's unlikely I'll be losing any significant amount of weight (enter possible menopause effects), I want to err on the side of a little bit larger so they stay proportional to the rest of my body.
So, now we wait, and prepare as much as we can for surgery, learn about recovery (which will be between 4 and 8 weeks), and brace ourselves for this next hill in the rollercoaster of a year we've had. I'm very thankful to Ben and his complete support in this process, who does not care ONE BIT what kind of surgery I decided to do--as long as I am comfortable with it.

And ultimately, I am comfortable with this plan. It doesn't remove all worry of recurrence, but nothing would. If the cancer wants to come back, it's going to find a way to come back and there's nothing any of us can do about that. But it won't be for lack of trying to beat it down and cut it out.
Triple negative breast cancer in a localized region after treatment generally has a 91% 5-year survival rate. And actually, my specific MammaPrint results put my 5-year survival percentage at 93% with hormone therapy and chemotherapy treatment. Since my cancer also had a small percentage of estrogen positive receptors, I'll also likely be taking an anti-estrogen hormone treatment pill called Tamoxifen for 5-10 years to prevent any estrogen-fed cancer cells from returning. The good news is that after 5 years, if it hasn't come back, the survival rate increases. Most triple negative cancers will recur within 3-5 years if they recur.
So, we are throwing everything we can at it, and trusting that God is in control and whatever the outcome is, we will handle it, because He'll guide us through it.












0 comments so far:
Post new comment